Uterine leiomyomas, commonly known as fibroids, are well-circumscribed, non-cancerous tumors arising from the myometrium (smooth muscle layer) of the uterus. In addition to smooth muscle, leiomyomas are also composed of extracellular matrix (i.e., collagen, proteoglycan, fibronectin). Other names for these tumors include fibromyomas, fibromas, myofibromas, and myomas.
Leiomyomas are the most common solid pelvic tumor in women, causing symptoms in approximately 25% of reproductive age women. However, with careful pathologic inspection of the uterus, the overall prevalence of leiomyomas increases to over 70%, because leiomyomas can be present but not symptomatic in many women. The average affected uterus has six to seven fibroids.
Leiomyomas are usually detected in women in their 30's and 40's and will shrink after menopause in the absence of post-menopausal estrogen replacement therapy. They are two to five times more prevalent in African American women than in Caucasian women. Risk for developing leiomyomas is also higher in women who are overweight or obese, but lower in women who have given birth. Although the high estrogen levels in oral contraceptive pills has led some clinicians to advise women with leiomyomas to avoid using them, there is some epidemiologic evidence to suggest that oral contraceptive use decreases the risk of leiomyomas.
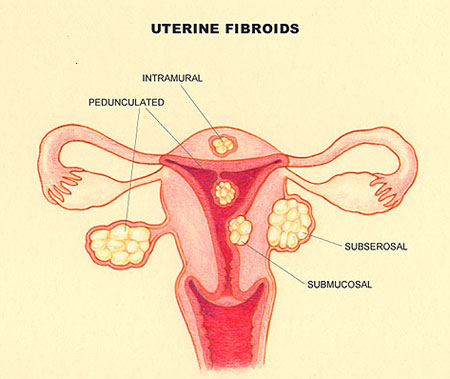
Leiomyomas are classified by their location in the uterus. Subserosal leiomyomas are located just under the uterine serosa and may be pedunculated (attached to the corpus by a narrow stalk) or sessile (broad-based). Intramural leiomyomas are found predominantly within the thick myometrium but may distort the uterine cavity or cause an irregular external uterine contour. Submucous leiomyomas are located just under the uterine mucosa (endometrium) and, like subserosal leiomyomas, may be either pedunculated or sessile. Tumors in subserosal and intramural locations comprise 95% of all leiomyomas; submucous leiomyomas make up the remaining 5%.
Leiomyomas are associated with a range of reproductive dysfunction, including recurrent pregnancy loss, infertility, premature labor, fetal malpresentations, and complications of labor. Although few studies exist regarding fibroid-related reproductive dysfunction, the prevailing clinical perspective is that these complications most often occur when fibroids physically distort the uterine cavity.
Therefore, women with large or symptomatic fibroids may choose to undergo assessment of the uterine cavity (such as by hysterosalpingography or by hysteroscopy) before attempting pregnancy. If fibroids are detected on the inside of the uterus (termed sub mucous fibroids) and distort the uterine lining, they may be a significant cause of reproductive problems and should be removed. It is less clear whether fibroids in the wall of the uterus cause reproductive problems. Generally, if the uterus is small, fibroids do not need to be removed in women contemplating or attempting pregnancy.
The diagnosis of leiomyomas can be easily determined by bimanual pelvic examination. During this routine office exam, the clinician evaluates the size and shape of the uterus and surrounding pelvic structures by inserting two fingers of one hand into the vagina while palpating the patient's abdomen above the pubic bone with the other hand. During this exam, a uterus with fibroids often feels enlarged and/or irregular, and may be felt abdominally above the pubic bone. In contrast, a non-pregnant uterus without fibroids is not palpable above the pubic bone.
In addition, imaging studies such as ultrasonography, MRI (magnetic resonance imagery), and CT (computed tomography) may be useful in confirming the diagnosis. Currently, ultrasonography is the most common method of confirming the diagnosis of leiomyomas.
There is no current medical treatment for fibroids. A myomectomy is a surgical procedure in which individual fibroid(s) are removed. Approximately 34,000 myomectomies are performed yearly in the United States. Most myomectomies are performed through an abdominal incision, although certain submucosal fibroids can be removed through the vagina without an abdominal incision during a procedure called hysterosopic myomectomy, which involves a special instrument called a hysteroscope. This technique is primarily useful for women with bleeding or pregnancy-related problems as there is usually little change in the size of the uterus with this approach. Certain subserosal fibroids may be removed abdominally during a procedure called laparoscopic myomectomy which involves a different instrument called a laparoscope. In general, myomectomy diminishes menorrhagia (prolonged and/or profuse menstrual flow) in roughly 80% of patients presenting with this symptom. Unfortunately, there is a significant risk of recurrence of fibroids after myomectomy; in some studies up to 10% of women who underwent an initial myomectomy required a second major operative procedure. In addition, 25-50% of women who underwent myomectomies had evidence by ultrasound of recurrence of their fibroids within one to ten years.
There are also several innovative techniques being studied as possible surgical treatment for fibroid-related bleeding. Myolysis involves delivering electric current via needles to a fibroid at the time of laparoscopy. Cryomyolysis involves using a freezing probe in a similar manner. Uterine artery embolization is a radiological alternative to surgery that involves placing a catheter into an artery in the leg and guiding the catheter via x-ray pictures to the arteries of the uterus. Once there, the catheter is used to deliver agents that block off these major blood vessels. While all of these treatments may prove to be effective treatments for fibroids when compared to more traditional options, the number of patients treated by these methods has been small. The follow-up has been relatively short term, and the safety of these procedures in women desiring pregnancy has not been demonstrated